Understanding Epidural Injection Costs with Insurance
Insurance coverage for epidural injections varies depending on the type of injection and the specific insurance plan.
Types of Epidural Injections Covered by Insurance
- Caudal Epidural Injections: Injections into the caudal space, located at the base of the spine.
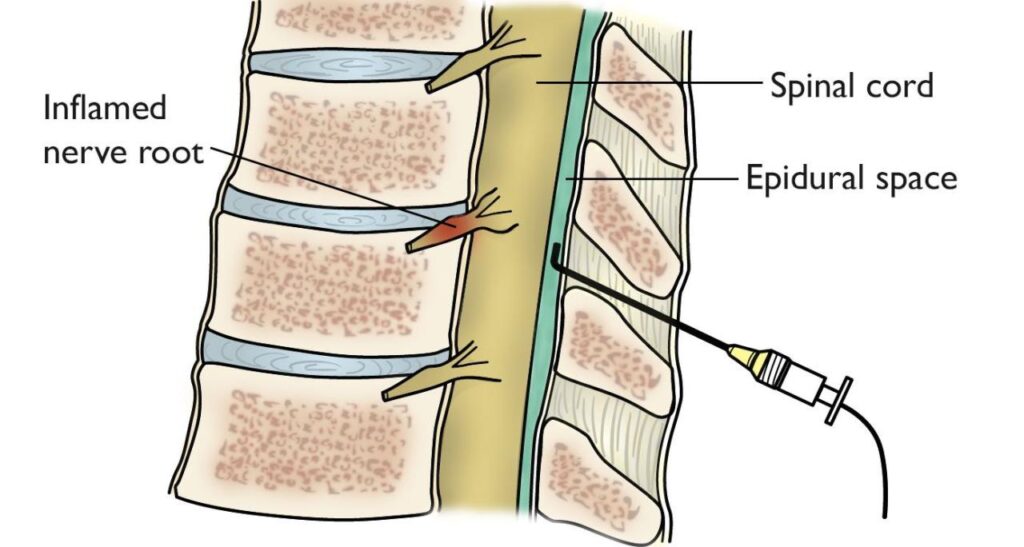
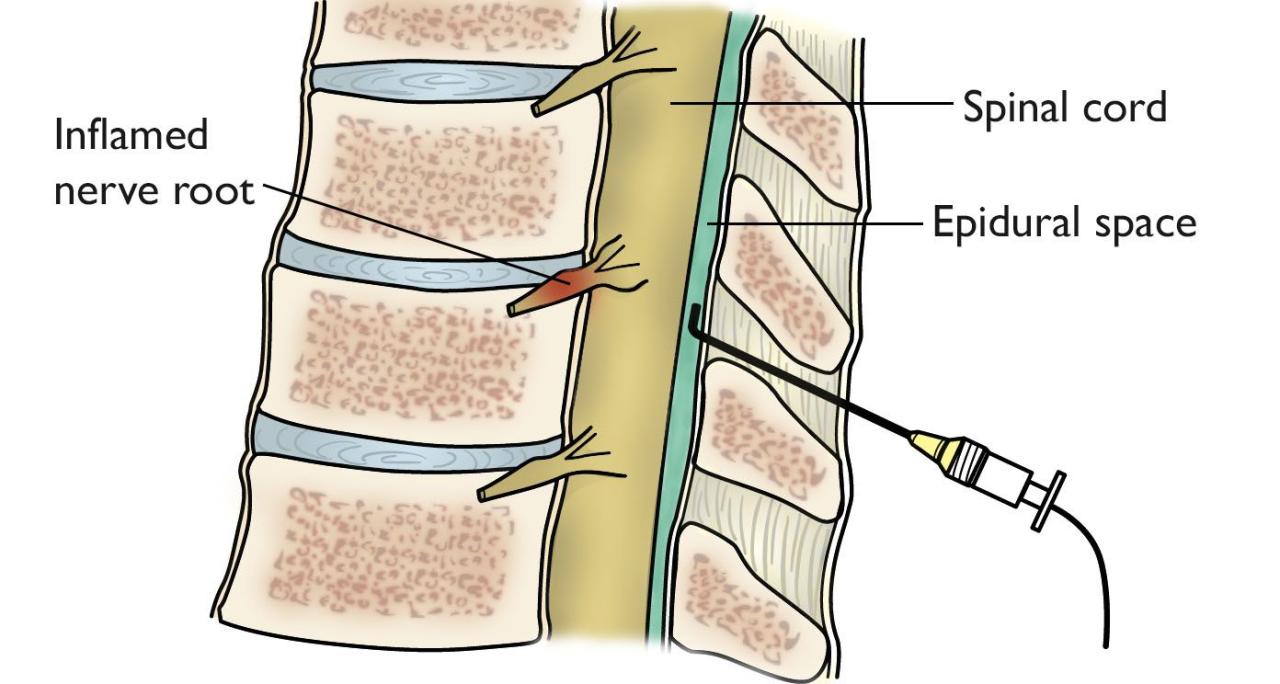
- Transforaminal Epidural Injections: Injections into the space around the nerve root, where it exits the spinal canal.
- Interlaminar Epidural Injections: Injections into the space between the vertebrae, where the spinal cord and nerves are located.
Average Costs of Epidural Injections with and Without Insurance
| Injection Type | Average Cost Without Insurance | Average Cost with Insurance |
|—|—|—|
| Caudal Epidural Injection | $1,000 – $2,000 | $200 – $500 |
| Transforaminal Epidural Injection | $1,500 – $2,500 | $300 – $600 |
| Interlaminar Epidural Injection | $1,200 – $2,200 | $250 – $550 |
Factors Influencing the Cost of Epidural Injections
- Type of Injection: Transforaminal injections are typically more expensive than caudal or interlaminar injections.
- Location of Injection: Injections in the cervical (neck) region are generally more expensive than injections in the lumbar (lower back) region.
- Provider: The cost of the injection may vary depending on the provider, such as a pain management specialist or anesthesiologist.
Coverage and Exclusions
Insurance coverage for epidural injections varies depending on the specific plan and policy. Generally, epidural injections are covered when they are medically necessary to treat certain conditions, such as back pain, neck pain, or sciatica.
To be eligible for coverage, the epidural injection must typically meet the following criteria:
- It must be performed by a qualified healthcare provider, such as a doctor or nurse practitioner.
- It must be performed in an approved medical setting, such as a hospital or clinic.
- It must be deemed medically necessary by the insurance company.
Common exclusions for epidural injections under insurance policies include:
- Injections that are performed for cosmetic purposes.
- Injections that are performed for experimental or investigational purposes.
- Injections that are performed for pain management without a clear medical diagnosis.
Out-of-Pocket Costs
Epidural injections can be expensive, and even with insurance, you may have to pay some out-of-pocket costs. The amount you pay will vary depending on your insurance plan, the type of epidural injection you receive, and the provider you see.
Calculating Out-of-Pocket Costs
To calculate your out-of-pocket costs, you will need to know your insurance plan’s deductible, coinsurance, and copay.
* Deductible: This is the amount you have to pay out-of-pocket before your insurance starts to cover the costs of your medical care.
* Coinsurance: This is the percentage of the cost of your medical care that you have to pay after you have met your deductible.
* Copay: This is a fixed amount that you have to pay for each medical service, such as an office visit or a prescription drug.
Once you know your insurance plan’s deductible, coinsurance, and copay, you can calculate your out-of-pocket costs for an epidural injection.
For example, if your insurance plan has a $1,000 deductible, a 20% coinsurance, and a $50 copay, you would have to pay the following out-of-pocket costs for an epidural injection that costs $2,000:
* Deductible: $1,000
* Coinsurance: $200
* Copay: $50
* Total out-of-pocket costs: $1,250
Tips for Reducing Out-of-Pocket Costs
There are a few things you can do to reduce your out-of-pocket costs for epidural injections.
* Negotiate with your provider. Some providers are willing to negotiate the cost of their services. If you are uninsured or have a high deductible, you may be able to get a discount on the cost of your epidural injection.
* Use a flexible spending account (FSA). An FSA is a tax-advantaged account that you can use to pay for qualified medical expenses, including epidural injections. Contributions to an FSA are made on a pre-tax basis, which means that you can save money on taxes.
* Consider getting a second opinion. If you are not sure whether an epidural injection is right for you, you may want to get a second opinion from another doctor. This can help you make an informed decision about your treatment and avoid unnecessary costs.
Billing and Coding
Epidural injections are billed using specific medical codes. The most common code is 62310, which covers the injection of medication into the epidural space. Other codes may be used depending on the specific type of injection performed.
Verifying Insurance Coverage
Before receiving an epidural injection, it’s crucial to verify your insurance coverage. Contact your insurance provider to determine if the procedure is covered and what your out-of-pocket costs may be.
Potential for Insurance Denials and Appeals
Insurance companies may deny coverage for epidural injections if they deem the procedure medically unnecessary or experimental. If your claim is denied, you have the right to appeal the decision. The appeals process typically involves submitting additional medical documentation and providing a written explanation of why the procedure is necessary.