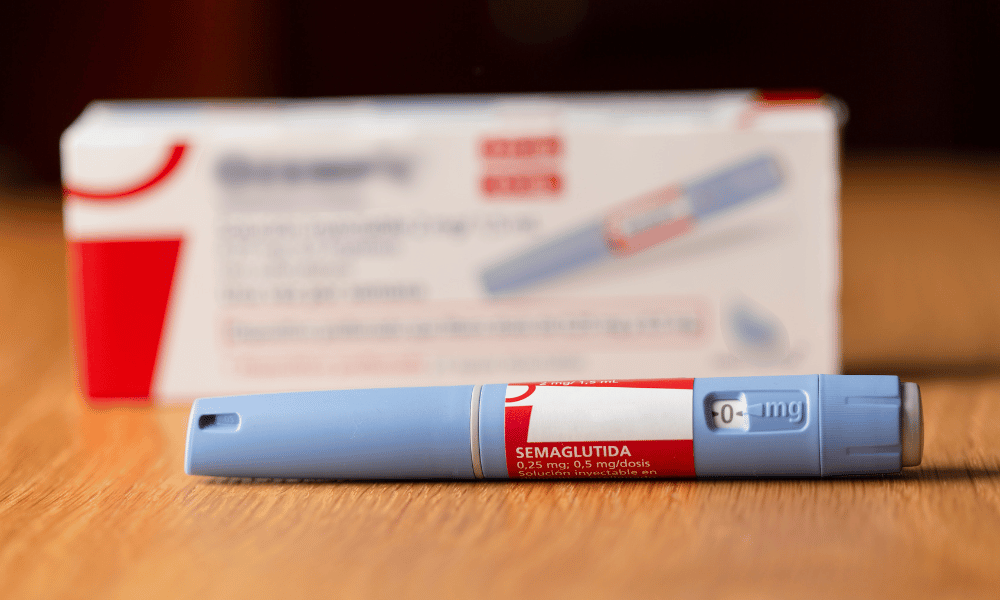
Ozempic Coverage for PCOS
Insurance coverage for Ozempic when prescribed for PCOS (Polycystic Ovary Syndrome) varies depending on the insurance provider and the specific plan.
Major insurance providers such as Cigna, UnitedHealthcare, and Aetna generally cover Ozempic for PCOS if it is prescribed by a healthcare professional for weight management in individuals with a BMI of 30 or higher, or a BMI of 27 or higher with at least one weight-related comorbidity such as high blood pressure or type 2 diabetes.
Successful Claims for Ozempic Coverage for PCOS
- A patient with PCOS and a BMI of 32 was prescribed Ozempic by their doctor. The patient’s insurance provider, Cigna, approved coverage for the medication after reviewing the patient’s medical records and confirming the diagnosis of PCOS and the need for weight management.
- Another patient with PCOS and a BMI of 28 and high blood pressure was prescribed Ozempic by their doctor. The patient’s insurance provider, UnitedHealthcare, also approved coverage for the medication after reviewing the patient’s medical records and confirming the diagnosis of PCOS and the presence of a weight-related comorbidity.
Denied Claims for Ozempic Coverage for PCOS
- A patient with PCOS and a BMI of 25 was prescribed Ozempic by their doctor. The patient’s insurance provider, Aetna, denied coverage for the medication because the patient’s BMI did not meet the criteria for coverage.
- Another patient with PCOS and a BMI of 30 was prescribed Ozempic by their doctor. The patient’s insurance provider, Humana, denied coverage for the medication because the patient did not have any weight-related comorbidities.
Criteria for Coverage
Insurance companies typically require specific diagnostic criteria and medical documentation to approve Ozempic coverage for PCOS. These criteria may vary depending on the insurance provider, but generally include:
A diagnosis of PCOS confirmed by a healthcare provider, supported by medical records documenting symptoms such as irregular menstrual cycles, elevated androgen levels, and polycystic ovaries on ultrasound.
Body Mass Index (BMI)
BMI is a measure of body fat based on height and weight. While BMI is not always an accurate indicator of overall health, insurance companies may consider BMI when determining coverage eligibility for Ozempic. Some insurance providers may require a BMI of 30 or higher (obese) or 27 or higher (overweight) with at least one weight-related comorbidity, such as type 2 diabetes or hypertension.
Prior Authorization Process
To obtain Ozempic coverage for PCOS, you may need to go through a prior authorization process. This process typically involves submitting a request to your insurance company for approval before the medication can be covered.
The prior authorization form usually requires information about your medical history, PCOS diagnosis, and treatment plan. You may also need to provide supporting documentation, such as a letter from your doctor explaining why Ozempic is medically necessary for your condition.
Tips for Completing the Prior Authorization Form
- Complete the form accurately and thoroughly, providing all the required information.
- Include a clear and concise explanation of your PCOS diagnosis and how Ozempic will help manage your condition.
- Attach supporting documentation from your doctor, such as a letter or medical records, to provide evidence of your medical necessity.
- Submit the form to your insurance company as early as possible to allow ample time for processing.
Appeals and Exceptions
If your insurance claim for Ozempic coverage for PCOS is denied, you have the right to appeal the decision. The appeals process typically involves submitting additional documentation and evidence to support your claim. You may also be required to attend a hearing to present your case.
There are also a number of exceptions that may be available to patients who do not meet standard coverage criteria. For example, some insurance companies may cover Ozempic for PCOS if the patient has tried and failed other treatments, or if they have a severe case of PCOS that is causing significant health problems.
Tips for Appealing a Denied Claim
* Gather all of your medical records and documentation related to your PCOS diagnosis and treatment.
* Write a letter to your insurance company explaining why you believe you should be covered for Ozempic.
* Be specific about how Ozempic will benefit you and how it will improve your quality of life.
* Include any supporting documentation from your doctor or other healthcare provider.
* Be prepared to attend a hearing to present your case.
Exceptions to Coverage Criteria
* Some insurance companies may cover Ozempic for PCOS if the patient has tried and failed other treatments.
* Some insurance companies may cover Ozempic for PCOS if the patient has a severe case of PCOS that is causing significant health problems.
* Some insurance companies may cover Ozempic for PCOS if the patient is enrolled in a clinical trial.
Alternative Medications
If Ozempic is not covered by your insurance for PCOS, several alternative medications may be available. These alternatives may include oral medications, injectables, or lifestyle modifications.
The efficacy and side effects of these alternatives vary depending on the individual and the specific medication. It’s important to discuss the benefits and risks of each option with your doctor to determine the best course of treatment for your specific needs.
Oral Medications
- Metformin: This medication is commonly used to treat type 2 diabetes and can also be effective in managing PCOS symptoms such as irregular periods, acne, and weight gain.
- Clomid (clomiphene citrate): This medication is used to stimulate ovulation in women with PCOS who are trying to conceive.
- Birth control pills: These medications can help regulate hormones and improve symptoms such as irregular periods, acne, and excessive hair growth.
Injectables
- Gonadotropins: These medications are used to stimulate ovulation in women with PCOS who are trying to conceive.
- GnRH agonists: These medications are used to suppress ovulation and can be effective in managing symptoms such as heavy bleeding and pain.
Lifestyle Modifications
- Weight loss: Losing even a small amount of weight can improve PCOS symptoms.
- Exercise: Regular exercise can help improve insulin sensitivity and reduce PCOS symptoms.
- Diet: Eating a healthy diet that is low in refined carbohydrates and sugar can help manage PCOS symptoms.
Financial Assistance Programs
If you are unable to afford the cost of Ozempic, several financial assistance programs are available to help you.
Eligibility criteria and application procedures vary depending on the program. To find out if you qualify for assistance, contact the manufacturer of Ozempic, Novo Nordisk, or a patient assistance organization.
Novo Nordisk Patient Assistance Program
Novo Nordisk offers a patient assistance program that may provide free or low-cost Ozempic to eligible patients. To qualify, you must meet the following criteria:
- Be a U.S. resident
- Have commercial insurance with a high deductible or coinsurance
- Meet certain income requirements
To apply for the Novo Nordisk Patient Assistance Program, you can call 1-800-727-6500 or visit their website at www.novonordisk-us.com/our-company/patient-assistance-programs.html.
Patient Assistance Organizations
Patient assistance organizations (PAOs) are non-profit organizations that provide financial assistance to patients who cannot afford their medications. To find a PAO that can help you with Ozempic, you can visit the following websites:
- Patient Access Network Foundation: www.panfoundation.org
- Partnership for Prescription Assistance: www.pparx.org
- NeedyMeds: www.needymeds.org